SAGES ANNUAL MEET, DALLAS,USA 2006
Complications of Surgery–P213
COMPLICATIONS OF LAPAROSCOPIC CHOLECYSTECTOMY TODAY- A REVIEW OF THE LITERATURE.- MANMOHAN VARMA MS, PRIVATE -
KANPUR, INDIA
OBJECTIVES: Laparoscopic cholecystectomy (LC) has emerged prominently in treatment of gallstone. Annually 770,000 procedures are performed
in USA alone. Complications have also changed. Thus it is prudent to review the literature on these complications. METHODS: Medline & PubMed
search was done for literature on the complications of LC till August 2005; its analysis is presented. RESULTS: Bile duct injury (BDI) is the scourge
of LC. Main cause is misperception & not lack of knowledge, skill or judgment. Misperception is so compelling that the problem is not recognized & is
an inherent risk of LC. Only 25% BDI are found peroperatively. Its incidence is 0.5% to 1.4% (few 2.7%). It is more severe & life-threatening. Mortality
& major morbidity after BDI were 12.1% & 30.3% respectively in a series of 13718 LCs. It has great impact on patient's physical & mental QOL. Some
need liver transplant. Beyond the learning curve, rate of BDI is still stable with significant legal & financial implications. But BDI is lesser at many
tertiary centers (0% in one). Nonbiliary damage is as frequent & devastating. Bleeding (mortality up to 0.2%) occurs from trocar sites or injury to
aorta, right hepatic artery (in 32% of BDI) & right external iliac artery. Stone spillage is 5% - 40% with problems in 7.0% like infection, abscess,
inflammation, adhesions, skin sinuses, bowel obstruction, pneumonia, cholelithoptysis, septicemia & middle colic vessel erosion. Added are bowel
injuries (up to 0.87%); diaphragmatic injury; portal vein injury; pseudoaneurysm of right hepatic artery; ilio-iliac arteriovenous fistula; liver laceration;
hemobilia; portal vein thrombosis; increased thromboembolism; large pneumothorax; huge surgical emphysema; clip migration led CBD stone; hernia
through falciform ligament defect with bowel obstruction; port site metastasis, TB & hernia. Pneumoperitoneum morbidity is up to 0.2%. Gas
embolism is rare & can kill. Anesthetic hazards need specific care. Limited information on litigations after LC favor surgeons in only 17.3%.
CONCLUSION: Complications of LC make it maximally invasive with only superficial small scars. Gallstone, a very common benign disease, does not
deserve risks of LC routinely. LC should be restricted to surgeons trained, experienced & working in tertiary hospitals. This would protect other
surgeons from lawsuits & undue stress of avoidable competition in surgical practice. Costs of LC's complications to healthcare system would reduce
too.
This paper, along with recent updates, has also been presented at 11th World Congress of Endoscopic Surgery, Yokohama, Japan 2008.
For Surgeons:
Bibliography of the above complications is available as ready reference. Please CLICK HERE.
This can then be used for defence in court of law since even most judges do not know that the laparoscopic surgeon's skill,
experience and judgment are usually not responsible for complications during Laparoscopic cholecystectomy.
The SINGLE HOLE SURGERY (LAIOUSC) described in this website has been designed to protect the patients against the
possibilities of these complications of 4 hole surgery (LC) while giving them the advantages of minimally invasive surgery. It
also is advantageous for surgeons as they shall not be burdened by:
1. Inherent and unpredictable complications of a procedure
2. Complications not detectable during surgery - as in many cases of bile duct injury.
Complications of Surgery–P213
COMPLICATIONS OF LAPAROSCOPIC CHOLECYSTECTOMY TODAY- A REVIEW OF THE LITERATURE.- MANMOHAN VARMA MS, PRIVATE -
KANPUR, INDIA
OBJECTIVES: Laparoscopic cholecystectomy (LC) has emerged prominently in treatment of gallstone. Annually 770,000 procedures are performed
in USA alone. Complications have also changed. Thus it is prudent to review the literature on these complications. METHODS: Medline & PubMed
search was done for literature on the complications of LC till August 2005; its analysis is presented. RESULTS: Bile duct injury (BDI) is the scourge
of LC. Main cause is misperception & not lack of knowledge, skill or judgment. Misperception is so compelling that the problem is not recognized & is
an inherent risk of LC. Only 25% BDI are found peroperatively. Its incidence is 0.5% to 1.4% (few 2.7%). It is more severe & life-threatening. Mortality
& major morbidity after BDI were 12.1% & 30.3% respectively in a series of 13718 LCs. It has great impact on patient's physical & mental QOL. Some
need liver transplant. Beyond the learning curve, rate of BDI is still stable with significant legal & financial implications. But BDI is lesser at many
tertiary centers (0% in one). Nonbiliary damage is as frequent & devastating. Bleeding (mortality up to 0.2%) occurs from trocar sites or injury to
aorta, right hepatic artery (in 32% of BDI) & right external iliac artery. Stone spillage is 5% - 40% with problems in 7.0% like infection, abscess,
inflammation, adhesions, skin sinuses, bowel obstruction, pneumonia, cholelithoptysis, septicemia & middle colic vessel erosion. Added are bowel
injuries (up to 0.87%); diaphragmatic injury; portal vein injury; pseudoaneurysm of right hepatic artery; ilio-iliac arteriovenous fistula; liver laceration;
hemobilia; portal vein thrombosis; increased thromboembolism; large pneumothorax; huge surgical emphysema; clip migration led CBD stone; hernia
through falciform ligament defect with bowel obstruction; port site metastasis, TB & hernia. Pneumoperitoneum morbidity is up to 0.2%. Gas
embolism is rare & can kill. Anesthetic hazards need specific care. Limited information on litigations after LC favor surgeons in only 17.3%.
CONCLUSION: Complications of LC make it maximally invasive with only superficial small scars. Gallstone, a very common benign disease, does not
deserve risks of LC routinely. LC should be restricted to surgeons trained, experienced & working in tertiary hospitals. This would protect other
surgeons from lawsuits & undue stress of avoidable competition in surgical practice. Costs of LC's complications to healthcare system would reduce
too.
This paper, along with recent updates, has also been presented at 11th World Congress of Endoscopic Surgery, Yokohama, Japan 2008.
For Surgeons:
Bibliography of the above complications is available as ready reference. Please CLICK HERE.
This can then be used for defence in court of law since even most judges do not know that the laparoscopic surgeon's skill,
experience and judgment are usually not responsible for complications during Laparoscopic cholecystectomy.
The SINGLE HOLE SURGERY (LAIOUSC) described in this website has been designed to protect the patients against the
possibilities of these complications of 4 hole surgery (LC) while giving them the advantages of minimally invasive surgery. It
also is advantageous for surgeons as they shall not be burdened by:
1. Inherent and unpredictable complications of a procedure
2. Complications not detectable during surgery - as in many cases of bile duct injury.
| SINGLE HOLE SURGERY FOR GALL BLADDER STONE |
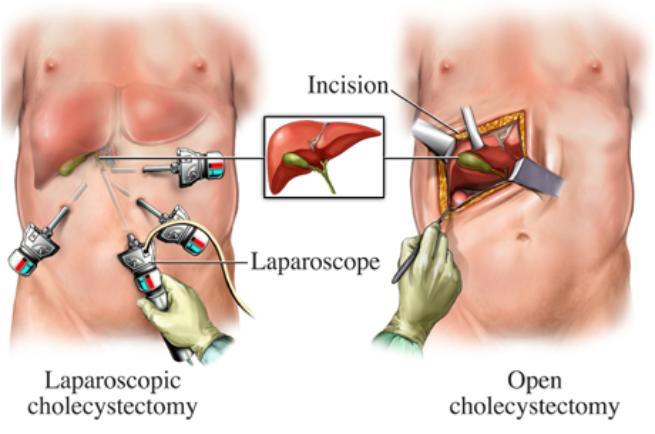
1. Open gall bladder surgery is much safer than 4 key hole surgery called Laparoscopic surgery for gall bladder, this
is because in 4 hole surgery the incidence of serious / life threatening complications is significantly higher. Thus we
are trading safety with comfort if opting for 4 hole surgery. The caution while choosing for 4 hole surgery is that it
should be got done at a recognized tertiary hospital where trained & qualified surgeons perform the operation and
not at any or every center that claims to perform this surgery. When a common man suffers no one notices it but
when a person of importance dies due to 4 hole surgery then doctors defend by saying that 4 hole surgery is riskier
& difficult while open surgery is safer. Please see the medical bulletin below on death of a senior senator in USA
after he underwent 4 hole surgery ... this surgery was got done at one of the established centers in USA. Although
surgeons performing 4 hole surgery will be all praise for it but the consent form that the patient has to sign will
mention all possible grave complications. For knowledge & safety: Please read the analysis at bottom of this page.
2. That there is now a well established SINGLE HOLE SURGERY technique for gall bladder removal. This is also a
laparoscopic surgery. Many surgeons who cannot do single hole surgery will dissuade the patient against it. This
surgery can be viewed at various links by putting "single hole surgery" in Google search. Two common links are :
http://www.sils.com/gallbladder/pages.aspx please read patient risk information at bottom of the page.
http://en.wikipedia.org/wiki/Single_port_laparoscopy
3. Gall Bladder Stone is a benign disease - meaning thereby that it is not a cancer.
4. Gall Bladder Surgery has certain complications: some are non life threatening while others are grave.
5. Traditional open surgery for gall bladder even today has statistically lesser grave type of complications of gall
bladder surgery compared to the 4 hole surgery called Laparoscopic Cholecystectomy (LC).
6.LC was introduced into medical science without the acceptable norms of double blind control trials and caused an
enormous increase in the incidence of common bile duct injuries which had grave consequences in many patients
including death.
7. Even after the learning curve the latest available overall data from SAGES* states that the over all common bile
duct injury rate is still very high. 1.4% as compared to 0 to 0.1% in open cholecystectomy.
*SAGES: SOCIETY OF AMERICAN GASTROINTESTINAL & ENDOSCOPIC SURGEONS
http://www.medscape.com/viewarticle/506432 states that:
The introduction of laparoscopic cholecystectomy (LC) in the late 1980s ushered in the era of minimally invasive
general surgery. Since then, it has become the preferred approach for cholecystectomy. During the initial years of
LC, when surgeons were in the "learning curve" of the procedure, there was a significant increase in bile duct
injuries (BDIs) compared with open cholecystectomy. However, most surgeons are now past their learning curve,
and many consider LC to be a "basic" laparoscopic procedure. Nevertheless, with the current incidence of BDIs as
high as 1.4%,[1,2] these injuries continue to be very morbid complications that have significant legal and financial
implications.
8. More than 770,000 cholecystectomies (gall bladder removal surgery) are done annually in USA and
approximately an equal number in Europe, making it a very common surgical procedure.
Thus some 10780 are suffering common bile duct injuries annually in USA and an equal number in Europe.
9. That beyond these injuries an equal number of other grave injuries occur during Laparoscopic surgery for gall
bladder removal. That even such injuries are caused which are never even possible in open surgery for gall bladder
removal.
10. Hernia from port sites is a common post operative occurrence in 4 hole surgery particularly in subsequent
pregnancy. This may need another surgery for repair / immediate surgery if complicated.
11. That to avoid injury to bile ducts a part of gall bladder called cystic duct was advocated to be left inside the
patient. This part is always removed in open surgery to prevent reformation of another sac called pseudo gall
bladder which can cause stones, colic and other problems.
12. That these complications are an inherent part of the surgical procedure and it is mostly NOT the surgeon’s fault
since the surgeon uses best of his judgment to deliver safe surgery to the patient. It is well documented in the
literature that bile duct injury is inherent to Laparoscopic surgery for gall bladder removal and not a lack of skill,
experience of judgment on part of the surgeon.
SURGICAL ENDOSCOPY Vol 20 Number 11 NOV 2006 has devoted its editorial & first 5 articles to the BILE DUCT INJURIES
caused during LAPAROSCOPIC CHOLECYSTECTOMY
is because in 4 hole surgery the incidence of serious / life threatening complications is significantly higher. Thus we
are trading safety with comfort if opting for 4 hole surgery. The caution while choosing for 4 hole surgery is that it
should be got done at a recognized tertiary hospital where trained & qualified surgeons perform the operation and
not at any or every center that claims to perform this surgery. When a common man suffers no one notices it but
when a person of importance dies due to 4 hole surgery then doctors defend by saying that 4 hole surgery is riskier
& difficult while open surgery is safer. Please see the medical bulletin below on death of a senior senator in USA
after he underwent 4 hole surgery ... this surgery was got done at one of the established centers in USA. Although
surgeons performing 4 hole surgery will be all praise for it but the consent form that the patient has to sign will
mention all possible grave complications. For knowledge & safety: Please read the analysis at bottom of this page.
2. That there is now a well established SINGLE HOLE SURGERY technique for gall bladder removal. This is also a
laparoscopic surgery. Many surgeons who cannot do single hole surgery will dissuade the patient against it. This
surgery can be viewed at various links by putting "single hole surgery" in Google search. Two common links are :
http://www.sils.com/gallbladder/pages.aspx please read patient risk information at bottom of the page.
http://en.wikipedia.org/wiki/Single_port_laparoscopy
3. Gall Bladder Stone is a benign disease - meaning thereby that it is not a cancer.
4. Gall Bladder Surgery has certain complications: some are non life threatening while others are grave.
5. Traditional open surgery for gall bladder even today has statistically lesser grave type of complications of gall
bladder surgery compared to the 4 hole surgery called Laparoscopic Cholecystectomy (LC).
6.LC was introduced into medical science without the acceptable norms of double blind control trials and caused an
enormous increase in the incidence of common bile duct injuries which had grave consequences in many patients
including death.
7. Even after the learning curve the latest available overall data from SAGES* states that the over all common bile
duct injury rate is still very high. 1.4% as compared to 0 to 0.1% in open cholecystectomy.
*SAGES: SOCIETY OF AMERICAN GASTROINTESTINAL & ENDOSCOPIC SURGEONS
http://www.medscape.com/viewarticle/506432 states that:
The introduction of laparoscopic cholecystectomy (LC) in the late 1980s ushered in the era of minimally invasive
general surgery. Since then, it has become the preferred approach for cholecystectomy. During the initial years of
LC, when surgeons were in the "learning curve" of the procedure, there was a significant increase in bile duct
injuries (BDIs) compared with open cholecystectomy. However, most surgeons are now past their learning curve,
and many consider LC to be a "basic" laparoscopic procedure. Nevertheless, with the current incidence of BDIs as
high as 1.4%,[1,2] these injuries continue to be very morbid complications that have significant legal and financial
implications.
8. More than 770,000 cholecystectomies (gall bladder removal surgery) are done annually in USA and
approximately an equal number in Europe, making it a very common surgical procedure.
Thus some 10780 are suffering common bile duct injuries annually in USA and an equal number in Europe.
9. That beyond these injuries an equal number of other grave injuries occur during Laparoscopic surgery for gall
bladder removal. That even such injuries are caused which are never even possible in open surgery for gall bladder
removal.
10. Hernia from port sites is a common post operative occurrence in 4 hole surgery particularly in subsequent
pregnancy. This may need another surgery for repair / immediate surgery if complicated.
11. That to avoid injury to bile ducts a part of gall bladder called cystic duct was advocated to be left inside the
patient. This part is always removed in open surgery to prevent reformation of another sac called pseudo gall
bladder which can cause stones, colic and other problems.
12. That these complications are an inherent part of the surgical procedure and it is mostly NOT the surgeon’s fault
since the surgeon uses best of his judgment to deliver safe surgery to the patient. It is well documented in the
literature that bile duct injury is inherent to Laparoscopic surgery for gall bladder removal and not a lack of skill,
experience of judgment on part of the surgeon.
SURGICAL ENDOSCOPY Vol 20 Number 11 NOV 2006 has devoted its editorial & first 5 articles to the BILE DUCT INJURIES
caused during LAPAROSCOPIC CHOLECYSTECTOMY
| Do we know that: |
FULL TEXT ….. of the news: (comments in RED color) PLEASE READ THIS :
~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~
Death of Rep. John Murtha Highlights Limitations of Laparoscopic Cholecystectomy
Robert Lowes
February 9, 2010 — Laparoscopic cholecystectomy (LC) is one of the most common surgeries in the nation, but yesterday's death of Rep. John
Murtha (D-PA) points out the rare, but unique, risks of this high-tech procedure, which include lack of depth perception and limitations in inspecting
for operative damage.
Murtha died of major complications from LC at Virginia Hospital Center in Arlington. He had undergone an LC at the National Naval Medical Center
in Bethesda, Maryland, on January 28, and was admitted to Virginia Hospital Center 3 days later. Several news organizations have independently
reported that Rep. Murtha suffered an infection after his intestine was inadvertently cut during the cholecystectomy. Neither hospital, when contacted
byMedscape Medical News, would confirm the nature of the complication.
Medical authorities typically put the complication rate for LC at roughly 2%. A study published in the April 1995 issue of the Annals of Surgery, for
example, reported a morbidity rate of 1.9% for LC compared with 7.7% for open-field cholecystectomy. [This is where the problem is: the morbidity
rate is quoted here BUT the incidence of dangerous complications during LC (like bile duct injuries & others) is NOT mentioned in contrast to their
incidence in open surgery. Hence the public at large and doctors who are not gastosurgeons come to falsely believe that LC is less riskier than
open gall bladder surgery while reverse is the case. Bile duct injury rate is on an average 14 to 20 times higher in LC and the type of bile duct
injury is usually more grievous. It is not reported probably BUT if we research for death incidence for similar patient groups then LC is likely to have a
higher death rate as a consequence of surgery. Once this information is publicised, doctors performing LC will not be unnecessarily blamed for
complications caused during LC, as inherently the technique of LC is riskier than open surgery. A riskier operation cannot be propogated with the
poor surgeon facing all the incrimination for the outcome. On the contrary the surgeons should be immune to outcome if patient chooses the
riskier operation: LC]
Among LC complications, a nicked intestine is one of the least common, according to a study by Thomas McLean, MD, JD, published in July 2006 in
the Archives of Surgery. Dr. McLean, a staff thoracic surgeon at the Dwight D. Eisenhower Veterans Affairs Medical Center in Leavenworth, Kansas,
found that bowel injuries accounted for 2% of adverse events in LCs that triggered a malpractice suit. The leading cause of litigation — 78% — was
injury to the bile duct. Such bile duct injuries are more common in LC than open-field cholecystectomy, Dr. McLean told Medscape Medical News.
Intestinal injuries, he said, are usually caused by trocar insertion. "There may be as many as 5 [trocars] inserted. This tends to be feel-only."
The intestine also can be injured when a surgeon is trying to separate it from an inflamed gallbladder that has adhered to it, said Nathaniel Soper,
MD, chairman of the Department of Surgery at Northwestern University Feinberg School of Medicine, Chicago, Illinois. The pressure of the carbon
dioxide gas used to inflate the abdomen during LC can seal up intestinal punctures that leak only after the gas is gone, Dr. Soper told Medscape
Medical News. He noted that either the small or large intestine can be accidentally cut during LC, although the duodenum of the small intestine is the
more likely candidate because of its proximity to the gallbladder. It is not clear from published accounts which intestine of Murtha's was accidentally
cut. [Intestinal injury is extremely rare in open surgery and usually instantly recognized, repaired and the complications are avoided]
Limitations of Laparoscopic Vision
Dr. Soper said the risk for accidental cuts increases with the distorted, depthless vision of the laparoscope.
"You're dependent on a 2-dimensional image," said Dr. Soper. "Because the image is very magnified, you're looking only at a very small part of the
(surgical) field, and you don't have a normal sense of feel using 2-foot long instruments."
In contrast, surgeons performing an open-field cholecystectomy enjoy a direct, 3-dimensional, panoramic view, added Dr. McLean. That improved
view helps them not only avoid a scalpel accident but also spot any accidents that occur during surgery. In addition, if surgeons are worried about
inadvertently cutting an intestine, they can pick it up and gently squeeze it to check for a leak. [ Despite the above facts surgeons performing LC are
expected to give results as less risky as in open surgery.. but this is unfair. Patients choosing a riskier operation should know, agree and accept the
outcome of LC as it is a surgery with its limitations as well as risks.]
Another risk factor for accidental intestinal cuts is obesity. In noting that the intestines can be injured during LC, the American College of Surgeons
states on its Web site that "patients who are obese...make it more difficult to move and manipulate instruments." However, an open-field
cholecystectomy for a morbidly obese person carries its own special risk — an incision that can be double the normal length, noted Dr. Soper. [If the
incision is double the normal length in obese patients but saves the patients from fatal complications of a surgery like LC, then, the normal
preference would be for the safer surgery]
Rep. Murtha, who was 77 years old, had represented the 12th Congressional District in southwestern Pennsylvania since 1974. An ex-Marine and
Vietnam War combat veteran, he was chairman of the House Appropriations Subcommittee on Defense. [Unfortunately an enquiry has been set up
against the surgeons who operated upon Murtha, this is because LC is falsely projected as a very safe and elementary procedure although it is just
the opposite. The dexterity and compulsions of surgeons ... including financial compulsions... are keeping LC alive. If all surgeons are given the
option to choose between open surgery and LC while ensuring that they would be financially compensated equally every month - no matter how
many patients opt for open or LC..... THE TRUTH WILL COME TO FORE...... Ofcourse then the surgeons who choose LC will have to hold
themselves resposnsible for the outcomes. Then the number of surgeons in open group as well as the woes of surgeons in LC group....if at all any
are there in LC group......will bring to fore the facts about risks of Laparoscopic Cholecystectomy.]
~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~
Laparoscopic Cholecystectomy is a surgical procedure with inherent as well as unique limitations and reported
complications. The surgeons performing this procedure are themselves NOT at fault for causing complications that they
cannot avoid. These complications are integral part of Laparoscopic Cholecystectomy as evidenced in the news pasted
below:
complications. The surgeons performing this procedure are themselves NOT at fault for causing complications that they
cannot avoid. These complications are integral part of Laparoscopic Cholecystectomy as evidenced in the news pasted
below:

| "Although it has been 25 years since the introduction of laparoscopic cholecystectomy into clinical practice, biliary and other injuries continue to occur for this most common of operations". http://www.sages.org/meetings/calendar/event/ihpba-lunch-symposium-safe-cholecystectomy/ |
| IHPBA Lunch Symposium on Safe Cholecystectomy (2016) |
| 4 Hole Surgery - Laparoscopic Cholecystectomy is a surgery with "Inherant Risks" and surgeon is not at fault if unavoidable complications occur. This has called for: |
| The "Single Hole Surgery" developed by us does not have complications unique to this 4 hole surgery |